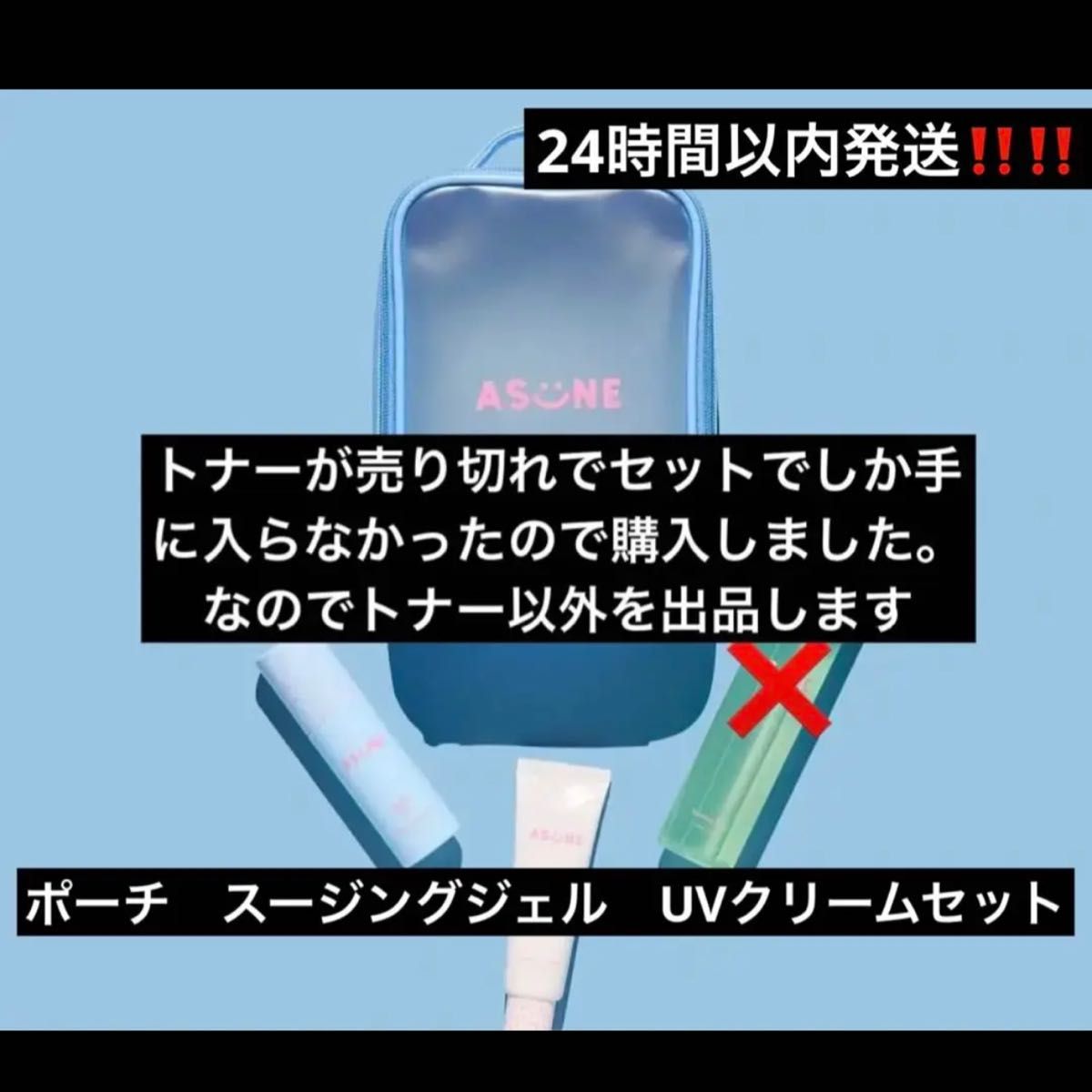
ASUNE Summer Pouch Set
(税込) 送料込み
商品の説明
間違えて2個購入したので出品します。
現在、完売している商品になります。
※即購入禁止商品の情報
| カテゴリー | コスメ・香水・美容 > スキンケア/基礎化粧品 > 化粧水/ローション |
|---|---|
| 商品の状態 | 新品、未使用 |

RESALE バンブートナー・ハートリーフマスク・サマーポーチ

2022年最新海外 アスネ ASUNE ◇ Summer ◇ サマーポーチセット Set

レア ASUNE Summer Pouch Set 化粧水/ローション - SOLUCENTERINT

金曜日までに売れなければ消去 中町綾 ASUNE Summer Pouch Set サマーポーチセット 値下げ不可

金曜日までに売れなければ消去 中町綾 ASUNE Summer Pouch Set サマーポーチセット 値下げ不可

ASUNE (@asune_official) • Instagram photos and videos

𝙑𝙞𝙩𝙖𝙢𝙞𝙣 𝙐𝙑 𝘾𝙧𝙚𝙖𝙢」&「𝘼𝙥𝙥𝙡𝙚 𝙎𝙤𝙤𝙩𝙝𝙞𝙣𝙜

Asuna -Undine- Summer Wedding ver. KADOKAWA Special Set

asune アップルスージングジェル - 通販 - hanackenovinky.cz

ASUNE 中町綾 バンブートナー UVクリーム

Kirby`s Dream Land School Bag (Set of 8) (Shokugan) - HobbySearch

asune アップルスージングジェル - 通販 - hanackenovinky.cz

Kirby`s Dream Land School Bag (Set of 8) (Shokugan) - HobbySearch

Amazon.com: The Summer Swan | Large Aesthetic Makeup Bag | Floral

Asuna -Undine- Summer Wedding ver. KADOKAWA Special Set
金曜日までに売れなければ消去 中町綾 ASUNE Summer Pouch Set サマーポーチセット 値下げ不可

Kirby`s Dream Land School Bag (Set of 8) (Shokugan) - HobbySearch

Amazon.com: The Summer Swan | Large Aesthetic Makeup Bag | Floral

Cos-Mart Lovelive AZUNA Osaka Shizuku/Uehara Ayumu/Yuki Setsuna Cosplay Costume Uniform Dress Activity Party Role Play Clothing

Hello Summer - POUCH

Kirby`s Dream Land School Bag (Set of 8) (Shokugan) - HobbySearch

Amazon.com: The Summer Swan | Large Aesthetic Makeup Bag | Floral

East Fabric Pouch Set of 2, Modern Autumn Season Wavy Holiday Festival Celebration Oriental Art Print, Small Drawstring Bag for Toiletries Masks and

yuuki sword art online | TOM Shop: Figures & Merch From Japan

Asuna -Undine- Summer Wedding ver. KADOKAWA Special Set

ASUNE(アスネ)|公式オンラインストア

ASUNE アスネ 中町綾 サマーポーチセット www.apidofarm.com

The Summer Swan | Large Aesthetic Makeup Bag | Floral Makeup Bag | Mid-day Clutch | Period Kit Bag | Hygiene Bag | Skincare Bag | Cute Makeup Bag
![AmiAmi [Character & Hobby Shop] |](https://img.amiami.com/images/product/review/232/FIGURE-153141_05.jpg)
AmiAmi [Character & Hobby Shop] |

Kirby`s Dream Land School Bag (Set of 8) (Shokugan) - HobbySearch
![AmiAmi [Character & Hobby Shop] |](https://img.amiami.com/images/product/review/232/FIGURE-153141_06.jpg)
AmiAmi [Character & Hobby Shop] |

Kirby`s Dream Land School Bag (Set of 8) (Shokugan) - HobbySearch

人気の贈り物が クランク FC-6700/6703/6750 172.5 パーツ - www

Amazon.com: The Summer Swan | Large Aesthetic Makeup Bag | Floral

Asuna Tea

Amazon.com: The Summer Swan | Large Aesthetic Makeup Bag | Floral

asune アップルスージングジェル - 通販 - hanackenovinky.cz

yuuki sword art online | TOM Shop: Figures & Merch From Japan

Tracksuit Women Sexy Club Outfit Jogging Full Female Sportswear Office Suit Crop Top And Pant Two Piece Set Home Clothes C5072

中町綾プロデュース〈 ASUNE (アスネ) 〉からベタつきが気になる肌を

商品の情報
メルカリ安心への取り組み
お金は事務局に支払われ、評価後に振り込まれます
出品者
スピード発送
この出品者は平均24時間以内に発送しています














