タイドラマ「The Shipper」Blu-ray
(税込) 送料込み
商品の説明
タイドラマ「The Shipper」Blu-ray
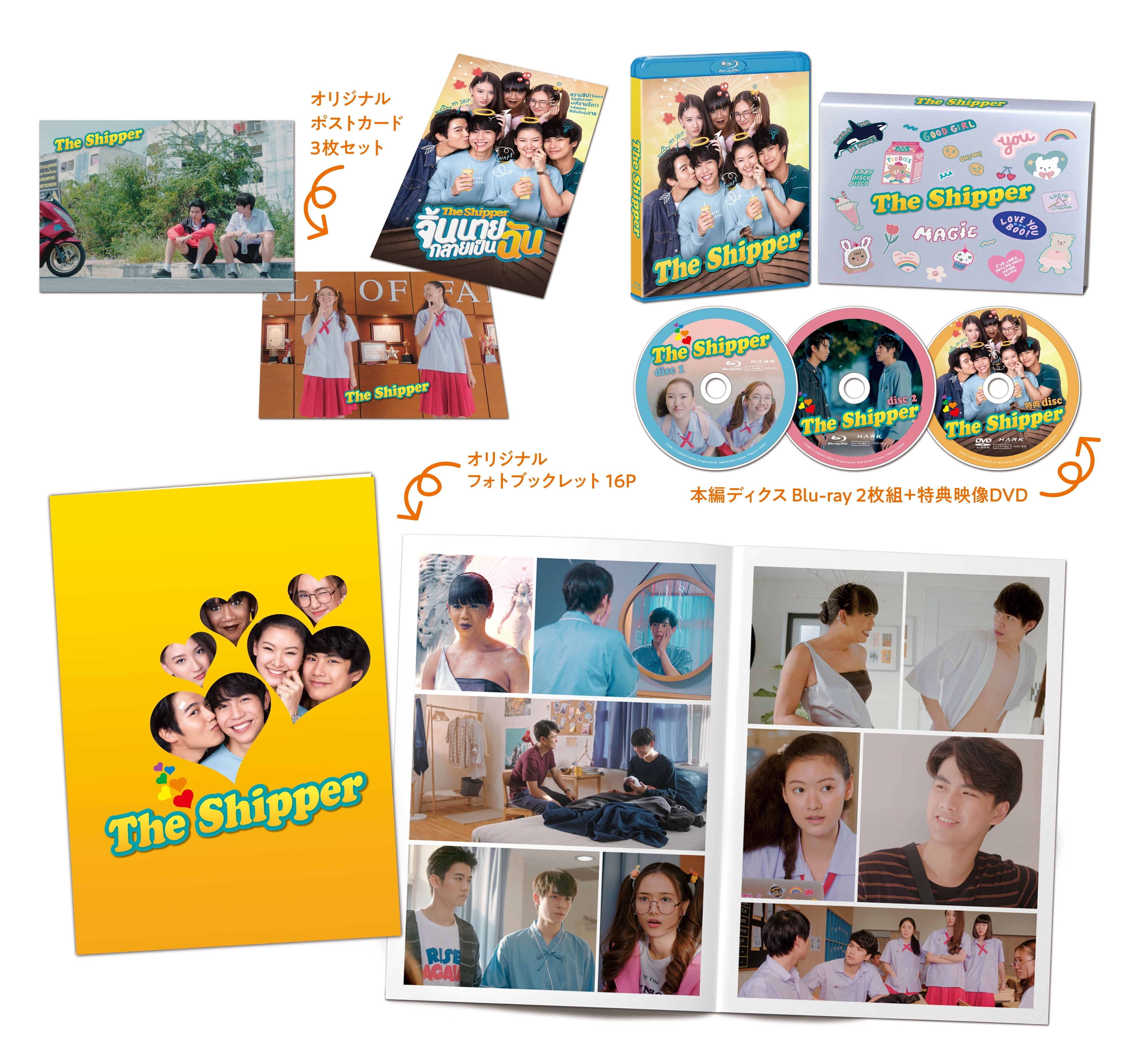
【内容】
本編BD2枚+特典DVD1枚+ポストカード3枚
各ディスク一度視聴し、暗所で保管していました。
タイドラマが好きな方にお譲りします。
即購入○
#タイドラマ
#GMMTV商品の情報
| カテゴリー | 本・音楽・ゲーム > DVD/ブルーレイ > TVドラマ |
|---|---|
| 商品の状態 | 目立った傷や汚れなし |
![Amazon | The Shipper [Blu-ray] -TVドラマ](https://m.media-amazon.com/images/I/811Dss70UDL._AC_UF894,1000_QL80_.jpg)
Amazon | The Shipper [Blu-ray] -TVドラマ

The Shipper」Blu-ray | ハーク オフィシャルショップ

新作在庫 お買い得 タイドラマ The Shipper Blu-ray aHS6Z
The Shipper」Blu-ray | ハーク オフィシャルショップ

新作在庫 お買い得 タイドラマ The Shipper Blu-ray aHS6Z

受注生産品】 The タイドラマ シッパー本編BD2枚+特典DVD1枚 ザ

タイドラマ fan BOOK! (晋遊舎ムック) |本 | 通販 | Amazon

The Shipper」Blu-ray | ハーク オフィシャルショップ

ヤフオク! -「タイドラマ dvd」(ブルーレイ) の落札相場・落札価格

<衛星劇場2021年03月>スペシャルプログラム タイドラマ 『The Shipper』 日本初放送 60秒予告
![Amazon | The Shipper [Blu-ray] -TVドラマ](https://images-fe.ssl-images-amazon.com/images/I/61HCH1QhROL._AC_UL600_SR600,600_.jpg)
Amazon | The Shipper [Blu-ray] -TVドラマ
タイBLドラマ:孤独な幽霊と大学生の切ないファンタジー・ラブ

2gether」GMMTVが贈るタイ青春ラブコメディ「The Shipper」衛星劇場

ドラマ「The Shipper」オフィシャルサイト

ヤフオク! -「タイドラマ dvd」(ブルーレイ) の落札相場・落札価格
![Amazon | The Shipper [Blu-ray] -TVドラマ](https://images-fe.ssl-images-amazon.com/images/I/81qdwZIUO L._AC_UL210_SR210,210_.jpg)
Amazon | The Shipper [Blu-ray] -TVドラマ

タイBLドラマ「The Shipper 」予告動画・あらすじ・出演者などの情報を

ギフト】 極美品TharnTypeターンタイプ 1・2(初回)Blu-rayBOXセット TV

タイドラマ the shipper ブルーレイ 全話の通販|ラクマ
ドラマ「The Shipper」オフィシャルサイト

The Shipper | 今月の新番組 | J:COM テレビ番組ガイド
![Amazon | The Shipper [Blu-ray] -TVドラマ](https://images-fe.ssl-images-amazon.com/images/I/91TwQyZcCSL._AC_UL600_SR600,600_.jpg)
Amazon | The Shipper [Blu-ray] -TVドラマ

タイドラマ「The Shipper」ロングTシャツ

衛星劇場2021年03月>スペシャルプログラム タイドラマ 『The Shipper
![YouTubeで視聴できるオススメタイBLドラマ[元気になる編] | 今、見て](https://melonchocoblog.com/wp-content/uploads/2023/05/41ef41dcdda6deef82daa00f8d1e3a4f.png)
YouTubeで視聴できるオススメタイBLドラマ[元気になる編] | 今、見て

Blu-ray TheShipper タイドラマ テレビドラマ | iesvegademijas.es

The Shipper 1話 | タイドラマファン❤

Blu-ray TheShipper タイドラマ テレビドラマ | iesvegademijas.es

The Shipper(韓流・アジアドラマ / 2020) - 動画配信 | U-NEXT 31日間

楽天ブックス: He's Coming To Me~清明節、彼は僕のお墓の隣に
![Amazon | The Shipper [Blu-ray] -TVドラマ](https://images-fe.ssl-images-amazon.com/images/I/917lDuHV9aS._AC_UL210_SR210,210_.jpg)
Amazon | The Shipper [Blu-ray] -TVドラマ

2gether」GMMTVが贈るタイ青春ラブコメディ「The Shipper」衛星劇場

ナイト・オブ・シャドー 魔法拳』Blu-ray | ハーク オフィシャルショップ
ドラマ「The Shipper」オフィシャルサイト

ヤフオク! - タイドラマ【 The Shipper 】☆全12話☆最高画...

Blu-ray TheShipper タイドラマ テレビドラマ | iesvegademijas.es

値引きする badboys Blu-ray j TVドラマ - store.barakatgallery.com

タイBLドラマ「The Shipper 」予告動画・あらすじ・出演者などの情報を

The Sipper が始まったよ!+『消えた初恋』 | タイドラマファン❤

TELASAタイドラマ特集 | Ohm×Nanon / Earth×Mixが明かす、世界中で愛さ





商品の情報
メルカリ安心への取り組み
お金は事務局に支払われ、評価後に振り込まれます
出品者
スピード発送
この出品者は平均24時間以内に発送しています














