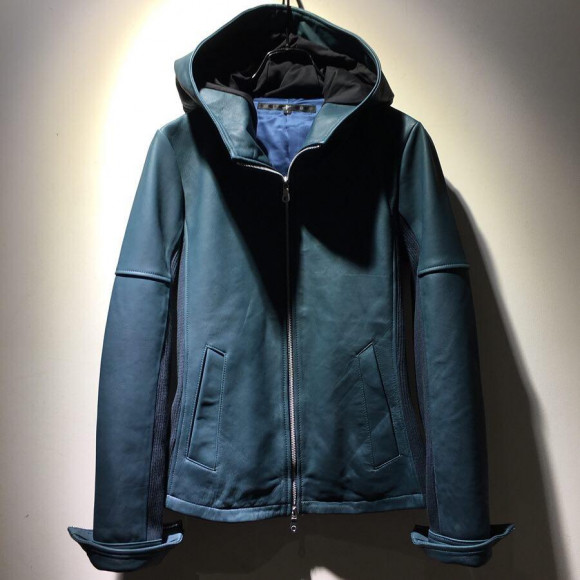
ラムバフィングフーデッドBLZ BLACK
(税込) 送料込み
商品の説明
NOID人気のレザー商品となります。
試着のみとなっておりますので
新品同様の美品となります。
現在は売り切れておりかなり貴重となります。
多少の値下げ⭕️
size1
色 BLACK商品の情報
| カテゴリー | メンズ > ジャケット/アウター > ライダースジャケット |
|---|---|
| 商品のサイズ | S |
| ブランド | ノーアイディー |
| 商品の状態 | 未使用に近い |

NO ID.OFFICIAL WEB STORE / ラムバフィングフーデッドBLZ

【NO ID.(ノーアイディー)】ラムバフィングフーデッドBLZ ブルゾン(844030-843L) | CAMBIO カンビオ

NO ID.(ノーアイディー)ラムバフィングフーデッドBLZブルゾン

NO ID. (ノーアイディー) ラムバフィングフーデッドBLZ ブルゾン ブラック サイズ:3

NO ID.OFFICIAL WEB STORE / ラムバフィングフーデッドBLZ

NO ID.OFFICIAL WEB STORE / ラムバフィングフーデッドBLZ

ラムバフィングフーデッドBLZ(ライダースジャケット)|NO ID

NO ID.OFFICIAL WEB STORE / ラムバフィングフーデッドBLZ

NO ID.(ノーアイディー)ラムバフィングフーデッドBLZブルゾン

新商品 NO 使い勝手の良い】 NO ID. ID ラムバフィングフーデッドBLZ

ジャケット ライダースジャケット ラムバフィングフーデッドBLZ

楽天市場】【NO ID.(ノーアイディー)】ラムバフィングフーデッドBLZ

ファッション 【NO ブルゾン ID.(ノーアイディー)】ラムバフィング

NO ID. official on X:

NO ID ラムバフィングフーデッドBLZ 早い者勝ち 7938円引き

NO ID.(ノーアイディ)の「ラムバフィングフーデッドBLZ(ライダース

【NO ID.(ノーアイディー)】ラムバフィングフーデッドBLZ ブルゾン(844030-843L)

NO ID.(ノーアイディー)】ラムバフィングフーデッドBLZ ブルゾン(844030-843L

ジャケット ライダースジャケット ラムバフィングフーデッドBLZ

NO ID.(ノーアイディー)ラムバフィングフーデッドBLZブルゾン

中古・古着通販】NO ID. (ノーアイディー) ラムバフィングフーデッド

楽天市場】【NO ID.(ノーアイディー)】ラムバフィングフーデッドBLZ
フーデッドレザージャケット | NO ID.・ショップニュース | 名古屋

☆大感謝セール】 public school カーキレザージャケット ジャケット

NOID ノーアイディー ラムバフィングフーデッドBLZ

ラムバフィングフーデッドBLZ/1/羊革/BLK/844030-843L

NO ID.(ノーアイディ)の「ラムバフィングフーデッドBLZ(ライダース

NO ID.OFFICIAL WEB STORE / ラムバフィングフーデッドBLZ

ジャケット ライダースジャケット ラムバフィングフーデッドBLZ
![NO ID.] LAMBバフィングフーデッドBLZ レザーパーカー 2 羊革 | www](https://img.fril.jp/img/486745134/l/1429476964.jpg)
NO ID.] LAMBバフィングフーデッドBLZ レザーパーカー 2 羊革 | www

NO ID.(ノーアイディー)ラムバフィングフーデッドBLZブルゾン

楽天市場】【NO ID.(ノーアイディー)】ラムバフィングフーデッドBLZ

開店祝い NO.ID ID.(ノーアイディー)ラムバフィングフーデッドBLZ

NO ID ラムバフィングフーデッドBLZ 早い者勝ち 7938円引き

新商品 NO 使い勝手の良い】 NO ID. ID ラムバフィングフーデッドBLZ

NO ID. ジャケット.Lambバフィングフーデッド比翼BLZ /ブラック/1 O-22

NO ID. フード付きラムレザージャケット ダブルジッパー 2022年新作

ラムバフィングフーデッドBLZ/1/羊革/BLK/844030-843L

NO ID. フーデッド ラムレザージャケット | vuzelia.com

NO ID.(ノーアイディ)の「ラムバフィングフーデッドBLZ(ライダース



商品の情報
メルカリ安心への取り組み
お金は事務局に支払われ、評価後に振り込まれます
出品者
スピード発送
この出品者は平均24時間以内に発送しています














